Abstract
Background
Research suggests racial/ethnic disparities in prenatal exposure to endocrine disrupting environmental phenols (EPs) in limited populations. However, no studies have investigated racial/ethnic disparities in prenatal EP exposure across the U.S.
Objectives
To estimate demographic differences in prenatal urinary EPs among participants in the Environmental influences on Child Health Outcomes (ECHO) Cohort.
Methods
An analysis of 4006 pregnant ECHO participants was performed, with 7854 specimens collected from 1999–2020. Racial/ethnic identity was self-reported. Urinary levels of 2,4-dichlorophenol (2,4-DCP), 2,5-dichlorophenol (2,5-DCP), benzophenone-3 (BP-3), bisphenols A (BPA), F (BPF), and S (BPS), and methyl- (MePb), ethyl- (EtPb), propyl- (PrPb), and butyl- (BuPb) parabens were measured at one or more time points during pregnancy. Effect estimates were adjusted for age, pre-pregnancy body mass index, educational level, gestational age and season at urine collection, and ECHO cohort.
Results
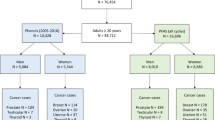
Participants were classified as Hispanic of any race (n = 1658), non-Hispanic White (n = 1478), non-Hispanic Black (n = 490), and non-Hispanic Other (n = 362), which included individuals of multiple races. Urinary 2,4-DCP and 2,5-DCP concentrations were 2- to 4-fold higher among Hispanic, non-Hispanic Black, and non-Hispanic Other participants relative to non-Hispanic White participants. MePb was ~2-fold higher among non-Hispanic Black (95% confidence interval (CI): 1.7–3.1) and non-Hispanic Other (95% CI: 1.5–2.8) participants. PrPb was similarly higher among non-Hispanic Black (95% CI: 1.7–3.7) and non-Hispanic Other (95% CI: 1.3–3.1) participants. EtPb was higher among non-Hispanic Black participants (3.1-fold; 95% CI 1.7–5.8). BP-3 was lower in Hispanic (0.7-fold; 95% CI: 0.5–0.9), non-Hispanic Black (0.4-fold; 95% CI: 0.3–0.5), and non-Hispanic Other (0.5-fold; 95% CI: 0.4–0.7) participants. Urinary BuPb, BPA, BPF, and BPS were similar across groups.
Impact statement
This multisite, observational cohort study investigated whether there are racial and ethnic differences in prenatal exposure to endocrine disrupting environmental phenols and parabens. Among 4006 participants from multiple U.S. cohorts who provided urine specimens during pregnancy, those who self-reported a racial and ethnic identity other than non-Hispanic White had higher urinary concentrations of 2,4-dichlorophenol, 2,5-dichlorophenol, methyl paraben, ethyl paraben, and propyl paraben and lower urinary concentrations of benzophenone-3 than those reporting as non-Hispanic White. These data show differences in prenatal concentrations of endocrine disrupting environmental phenols and parabens by racial and ethnic identity.
Similar content being viewed by others
Introduction
Gestational exposure to environmental endocrine disrupting chemicals (EDCs) is widespread [1, 2]. Environmental phenols (EPs), including parabens, are types of EDCs with reported estrogenic, anti-androgenic, and thyroid-hormone effects [3]. These chemicals are employed in the manufacture of polycarbonate plastics, food packaging, heat transfer papers like receipts, and medication, among other commercial products, and as ultraviolet filters and preservatives in sunscreens, personal care products, and processed foods as summarized in Supplementary Table 1 [4,5,6,7,8]. Exposure occurs through consumer items, food packaging, personal care products, and household dust [9, 10], and many EPs readily cross the placenta to expose the developing fetus [11]. Despite short in vivo half-lives, EPs are detected frequently in human biospecimens, underscoring their pervasive nature. Prenatal exposure to EPs has been associated with reproductive morbidities, infertility, adverse birth outcomes, altered fetal and child development, and long-term health risks among offspring, possibly partially accounting for poorer reproductive health outcomes among minoritized populations [12,13,14].
Results of U.S. biomonitoring studies, using data from the National Health and Nutrition Examination Survey, indicate that EP exposure tends to be disproportionately experienced by non-White and low-income groups in the general population [15,16,17,18,19]. Previous studies of urinary EPs among pregnant people in the U.S. have also reported racial, ethnic, and socioeconomic disparities in exposure to EPs [20,21,22,23,24]. Residents of socioeconomically disadvantaged and minoritized communities may experience greater risks of exposure to EPs than advantaged and non-Hispanic White communities, due to greater proximity to industry and waste management facilities, and a limited selection of consumer products and fresh foods [25]. However, these previous studies were limited in size and scope, mostly offering insight into the nature and extent of the exposure disparity on a local basis and/or did not consistently report racial/ethnic differences with adjustment for social determinants. No studies have comprehensively characterized the differences in concentrations of EPs among pregnant people with various self-reported racial and ethnic identities and across different regions of the U.S. [26].
We leveraged extant urinary gestational EP data from 11 cohorts across the U.S. and Puerto Rico within the Environmental Influences on Child Health Outcomes (ECHO) Cohort to help address this important public health data gap. Synthesizing results across multiple studies from different U.S. regions can help inform policy makers on target priorities to eliminate disparities in exposure to EDCs among pregnant populations at a large scale. We selected the EPs for study based on a high reported prevalence of exposure in U.S. study populations, evidence of endocrine disruption, and availability in the ECHO cohorts. We hypothesized that non-White pregnant people would have higher urinary concentrations of most EPs than their White counterparts, conditional on social determinants.
Methods
Study participants
The ECHO Cohort consists of mother–offspring pairs in 69 different birth cohorts from across the U.S. [27]. All participants completed written informed consent for participation in their cohorts and consented to data sharing with the ECHO program. We excluded cohorts with <30 eligible participants and participants were required to have at least one urine specimen collected during pregnancy, with laboratory determination of at least one EP, leaving 4139 participants from 11 ECHO cohorts (96.8% were singleton pregnancies, 3% were missing, and 0.2% were multiple gestations). We retained only singleton pregnancies. Thus, a total of 7854 urine specimens from 4006 participants from 11 ECHO cohorts were included in the final analytic sample (Supplementary Figs. 1 and 2; Supplementary Table 2). The study protocol was approved by the single ECHO institutional review board, WIRB Copernicus Group Institutional Review Board.
Sociodemographic characteristics
Participants self-reported their racial/ethnic identities, which we subsequently categorized as Hispanic of any race, non-Hispanic Black, non-Hispanic White, and non-Hispanic Other—a category that included non-Hispanic Asian, Hawaiian, American Indian, Alaskan Native, multiple races, and other racial identities (the small number of participants in each group precluded statistical analysis of the individual identities). Race is a social construct, used in this analysis as a proxy for individual and systematic lived experiences of racism and discrimination resulting from complex prior and ongoing historical processes based (primarily) on racial grouping [28, 29]. Participants also self-reported their highest completed level of education, used as a proxy for socioeconomic position [30]. Educational level was categorized as ≥bachelor’s degree and <bachelor’s degree based on differences in social advancement and lifetime earnings potential [31]. Home address was geocoded in a subset of participants and categorized using Social Vulnerability Index (SVI), a census tract-level composite indicator variable of neighborhood stressors that incorporates 16 measures of socioeconomic status, household characteristics, racial and ethnic minority status, and housing type and transportation [32].
Urinary EP measurements
Participants provided one or more urine specimens during pregnancy, which were analyzed for EPs by participating laboratories (Supplementary Table 2). We imputed chemical values measured below the limit of detection (LOD) as the LOD/√2 (Supplementary Table 3) [33]. Urine samples submitted to the different study laboratories were returned with either specific gravity or creatinine values. Every study participant had either a urinary specific gravity or urinary creatinine value reported. Depending on which was reported, a correction was applied to correct for differences in urinary dilution, by multiplying the measurement by the ratio of the creatinine or specific gravity in a reference population to the participant’s observed creatinine or specific gravity, respectively, using the Boeniger method [34], as recently recommended for combining cohorts with different measures of urinary dilution [35]. We considered the following EPs measured widely among participating cohorts and implicated as EDCs: 2,4-dichlorophenol (2,4-DCP), 2,5-dichlorophenol (2,5-DCP), benzophenone 3 (BP-3), bisphenol A (BPA), bisphenol F (BPF), bisphenol S (BPS), methyl paraben (MePb), ethyl paraben (EtPb), propyl paraben (PrPb), and butyl paraben (BuPb). Common routes and sources of exposure are summarized in Supplementary Table 1.
Data analysis
To estimate associations of racial/ethnic categories and educational level with urinary chemical concentrations, we applied linear mixed regression models with a censored normal distribution, including a random intercept for participants. Urine specimens were analyzed at different laboratories, employing different methods and instruments that had distinct LODs, so LOD values vary across the cohorts as shown in Supplementary Table 3. We used a censored regression model to help address this challenge in pooling the laboratory results from the different cohorts. Such models can accommodate varying left-censored observations lower than the LOD by partitioning the likelihood function into components predicting values lesser and greater than the LOD. Specifically, the model first creates an indicator variable that flags whether a measured value is below or above the LOD. This indicator variable is included in the model to appropriately account for differences in LOD across cohorts and optimization is either based on an expectation maximization algorithm or Gauss-Hermite quadrature [36, 37].
In all of the multivariable models, we adjusted for maternal highest education level, ECHO cohort, gestational age at specimen collection (in weeks), season of specimen collection, maternal age at specimen collection (in years), and maternal pre-pregnancy body mass index (in kg/m2) as fixed effects. Covariates were selected based on hypothesized relationships of racial/ethnic identity with urinary chemical concentrations according to the literature using a directed acyclic graph [38, 39] (Supplementary Fig. 3). We did not adjust for year of urine collection as it was colinear to study cohort. To evaluate effect measure modification in the pattern of associations, we stratified the educational level predictor model by racial/ethnic identity. To address the potential impact of neighborhood-level confounding and to disentangle influences of structural socioeconomic disadvantage from self-reported race/ethnicity, we performed sensitivity analyses in which we adjusted for SVI in a subsample of 2117 participants with a geocoded home address. To evaluate the influence of gestational age at urine collection, we performed sensitivity analyses using only second trimester data, which accounted for the majority of urine specimens collected. We also performed a leave-one-cohort-out analysis to assess the influence of individual ECHO cohorts.
We used multiple imputation by chained equations to impute missing covariates and pooled estimates from the imputed data sets using Rubin’s rules. During sensitivity analyses, the list of covariates adjusted in each model varied based on data availability. Stratifying the dataset exclusively to a specific race/ethnicity or educational level resulted in scenarios where certain variables did not exhibit variability and were excluded from the analysis. Furthermore, because of the unbalanced nature of repeated measurements, stratifying the dataset during sensitivity analyses resulted in datasets with one observation per subject or all observations above the LOD for certain strata. We used general linear or linear mixed effects models, respectively, in these scenarios. Statistical significance was defined as a 2-sided p < 0.05. We further adjusted the type-1 error rate using a conservative Bonferroni approach for the effective number of tests of each predictor, as 0.05/10 = 0.005 [40]. Statistical analyses were performed using R statistical software, v.4.2.2 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Sociodemographic characteristics of the participants
Study participants self-reported Hispanic (41.4%), non-Hispanic Black (12.2%), non-Hispanic Other (9.0%), and non-Hispanic White (36.9%) race and ethnicity (Table 1). Approximately half (46.8%) had completed a bachelor’s degree. The mean gestational age at urine collection was 20.1 weeks, with an interquartile range of 14–26 weeks.
Distributions of urinary EP concentrations
Ten urinary chemicals were measured in participants (Supplementary Table 4). Nine of the 10 EPs were detected in a majority of participants, except for BPF (40.31% > LOD). MePb had the highest median urinary concentration (58.56 µg/L), and BuPb had the lowest (0.16 µg/L). There were moderate to strong positive correlations among Log-transformed urinary EtPb, BuPb, MePb, and PrPb (r = 0.34-0.79), and between log-transformed urinary 2,4-DCP and 2,5-DCP (r = 0.58) (Supplementary Fig. 4). The distribution of urinary chemicals varied by ECHO cohort (Supplementary Fig. 5).
Boxplots of log-transformed urinary chemical concentrations are shown according to self-reported maternal racial/ethnic identity (Fig. 1). Non-Hispanic Black participants had higher urinary 2,4-DCP, 2,5-DCP, EtPb, MePb, and PrPb concentrations than participants with other racial/ethnic identities. Urinary BPA and BPS concentrations were highest among Hispanic participants, and BP-3 was highest among non-Hispanic White participants.
Associations between self-reported maternal racial/ethnic identity category and urinary EPs
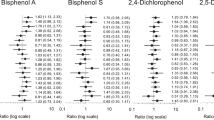
Figure 2 and Supplementary Table 5 show the covariate-adjusted associations between self-reported racial/ethnic identity and urinary chemicals. Relative to non-Hispanic White participants, Hispanic participants had 1.50-fold (95% confidence interval (CI): 1.20–1.87) and 4.07-fold (95% CI: 3.05–5.42) greater urinary 2,4-DCP and 2,5-DCP concentrations, respectively, but a 0.67-fold (95% CI: 0.52–0.85) lower urinary BP-3 level; non-Hispanic Black participants had 3.08-fold (95% CI: 2.22–4.27), 2.30-fold (95% CI: 1.73–3.06), 3.11-fold (95% CI: 1.66–5.82), and 2.55-fold (95% CI: 1.74–3.72) higher urinary 2,5-DCP, MePb, EtPb, and PrPb levels, respectively. Relative to non-Hispanic White participants, non-Hispanic Black participants had 0.38-fold (95% CI: 0.27–0.51) lower urinary BP-3 concentrations; non-Hispanic Other participants had 2.06-fold (95% CI: 1.42–2.99), 2.02-fold (95% CI: 1.46–2.80), and 2.01-fold (95% CI: 1.30–3.11) higher urinary 2,5-DCP, MePb, and PrPb levels, respectively, but a 0.49-fold (95% CI: 0.37–0.65) lower urinary BP-3 level.
Effect estimates are ratios of geometric means and 95% confidence intervals from individual linear mixed effect censored-response regression models of specific gravity/creatinine-corrected urinary phenol concentrations as outcomes and maternal racial and ethnic identity categories as predictors (non-Hispanic White = reference category), a random intercept on pregnancy to account for multiple urinary measurements and adjusted for maternal age (years), pre-pregnancy body mass index (kg/m2), educational level (completed vs. did not complete bachelor’s degree), gestational age at biospecimen collection (weeks), season of biospecimen collection (fall vs. winter vs. spring vs. summer), and ECHO study cohort (11 cohorts). Abbreviations: BPA bisphenol A, BPF bisphenol F, BPS bisphenol S, ECHO Environmental Influences on Child Health Outcomes, Mult/Oth/Asian non-Hispanic multiple races, “Other,” and Asian.
The results were similar, but somewhat attenuated, when we adjusted for the SVI in a sensitivity analysis of 2117 participants with a geocoded home address (Supplementary Table 6) and when we limited the analysis to urine specimens collected during the second trimester (Supplementary Table 7). The results of the leave-one-cohort-out analysis were mostly consistent with the main findings (Supplementary Fig. 6). However, exclusion of The Infant Development and Environment Study (TIDES) cohort changed the direction of the effect estimates, with urinary BPA concentrations similar between non-Hispanic Black and non-Hispanic White participants and lower among Hispanic and non-Hispanic Other participants than non-Hispanic White participants. There were also increases in the magnitude of the association of race/ethnic identity with BPF among Hispanic participants and with BPS among Hispanic, non-Hispanic Black, and non-Hispanic Other participants relative to non-Hispanic White participants when excluding the New York University Child Health and Environment Study (NYU-CHES) cohort.
Associations between maternal educational level and urinary EPs
Table 2 shows the associations between maternal educational level and urinary EPs, adjusted for covariates, according to maternal racial/ethnic identity. In all racial and ethnic groups, participants who had not completed a bachelor’s degree had lower urinary BP-3 than participants who had completed a bachelor’s degree or more, although with statistical significance only for Hispanic (0.68-fold; 95% CI: 0.55–0.84) and non-Hispanic Other (0.44-fold; 95% CI: 0.25–0.77) participants following the Bonferroni adjustment procedure. There was also a consistent pattern of higher urinary BPS and 2,5-DCP among participants who had not completed a bachelor’s degree in all racial and ethnic identity groups, although without statistical significance. Supplementary Table 8 shows a similar pattern of associations between maternal educational level and gestational urinary BP-3, BPS, and 2,5-DCP concentrations in the overall sample.
Discussion
In this investigation of 4006 pregnant ECHO participants, we found that average urinary EP concentrations differed by self-reported racial/ethnic identity. Non-Hispanic Black and Hispanic participants had greater average urinary concentrations of 2,5-DCP, the primary metabolite of paradichlorobenzene [4], than non-Hispanic White participants. Paradichlorobenzene is used in mothballs, fumigants, and room/toilet deodorizers, allowing the chemical to be inhaled [5]. It is neurotoxic and weakly antiestrogenic in rodents [41], and exposure has been associated with estrogen-sensitive cancers [42]. Urinary MePb, EtPb, and PrPb levels were also higher among non-Hispanic Black than non-Hispanic White participants. These chemicals are weakly estrogenic and used as preservatives in prepared foods and personal care products, allowing them to be ingested and absorbed [8]. Higher gestational exposure to MePb was associated with greater risks of adverse birth outcomes and attention-deficit hyperactivity disorder among offspring [43]. In contrast, average urinary concentrations of BP-3, a UV-filtering chemical absorbed from sunscreens and personal care products, were highest among non-Hispanic White participants. BP-3 has been found to be estrogenic in experimental models, and exposure was associated with adverse reproductive outcomes in human studies [6]. However, we found that the associations did not differ by educational attainment, suggesting that factors other than educational attainment, as a proxy for socioeconomic position, played an important role in racial/ethnic differences. Differential exposure may account in part for racial/ethnic differences in perinatal health outcomes.
Comparison with previous studies
Pregnant people from across the U.S. with racial and ethnic identities other than non-Hispanic White had higher urinary concentrations of most measured EPs than their non-Hispanic White counterparts. Our results are largely consistent with the results of several previous studies of pregnant people that have also reported racial and ethnic differences in urinary EPs among smaller samples of the U.S. population from limited areas [20,21,22,23,24]. Biomonitoring studies have also described similar racial and ethnic differences in urinary EPs among representative samples of the general U.S. population [19, 44,45,46]. However, unlike the general U.S. population samples that included people without pregnancy, children, and seniors, our study focused on pregnant people.
Similar to our results, the 2009–2010 U.S. National Children’s Study Vanguard Study (NCS) of 506 pregnant women (some of whom were included in this analysis) showed higher urinary 2,5-DCP levels among non-Hispanic Black than non-Hispanic White participants [20]. Urinary 2,5-DCP levels were similarly lowest among non-Hispanic White participants and those with the highest educational level in the 2009–2014 Healthy Start study of 446 pregnant women from Colorado (some of whom were included in this analysis) [21]. African Americans, a non-Hispanic Black group, had the highest urinary 2,4-DCP and 2,5-DCP levels in the 2006–2008 LIFECODES study of 480 pregnant women from Boston, Massachusetts [22]. These results are consistent with our own findings and with those from a representative sample of U.S. women from 1999–2014, for whom urinary concentrations of 2,4-DCP and 2,5-DCP levels were higher among non-Hispanic Black and Hispanic women than non-Hispanic White women [44]. Similar to the U.S. biomonitoring study, we did not find an association between urinary 2,4-DCP and 2,5-DCP and educational level [44].
In addition, our findings were consistent with results from a 2003–2004 study showing that U.S. non-Hispanic White participants had greater average urinary BP-3 than non-Hispanic Black and Mexican American participants [19]. Pregnant non-Hispanic White women had similarly higher urinary BP-3 concentrations than other racial/ethnic groups in the NCS and Healthy Start studies [20, 21], and BP-3 levels were positively correlated to educational level in the Healthy Start and LIFECODES studies [21, 22]. We also found higher BP-3 levels among pregnant people with more education.
BPA is a plastic monomer used in polycarbonate plastics, epoxy can linings, heat transfer papers, and other consumer goods [7]. BPA levels were similar across different racial/ethnic categories among U.S. women in 1999–2014 [44]. In contrast, urinary levels of BPS, a BPA-replacement chemical, were highest among non-Hispanic Black women, and urinary levels of BPF, another BPA replacement, were highest among non-Hispanic White women from 1999–2016; these differences could not be attributed to income as an indicator of socioeconomic position [44]. Urinary BPS and BPA were similarly highest among non-Hispanic Black U.S. adults from 2007–2016, but there was no significant difference in BPF; concentrations were greatest among those with the lowest education [45]. In contrast, urinary BPA levels were similar among 233 non-Hispanic White, Hispanic, and Other (including Asian, Black, and multiracial) pregnant California women enrolled in the Markers of Autism Risk in Babies–Learning Early Signs (MARBLES) study from 2007–2014, although those with less education had higher urinary BPA levels [23]. We did not find a statistically significant difference in urinary BPA, BPS, or BPF levels between racial/ethnic categories after the Bonferroni adjustment, although our results suggested higher urinary BPA among non-Hispanic Black compared to non-Hispanic White participants. We also did not find associations of BPA, BPF, or BPS with educational level. The differences between our results and those from U.S. biomonitoring data may in part reflect higher intraindividual variabilities in prior studies based on a single urine specimen [47] and different time-activity exposure patterns between pregnant and non-pregnant populations [48].
Our results were similar to those reported in a previous analysis of the Healthy Start Study, in which non-Hispanic Black participants and participants with other racial/ethnic identities had the highest urinary MePb, EtPb, and PrPb levels and non-Hispanic Black participants had the lowest urinary BuPb levels [21]. Higher education was related to higher urinary EtPb and PrPb levels in Healthy Start. Similarly, urinary MePb and PrPb levels were greatest among African American participants, whereas BuPb levels were greatest among White participants in the LIFECODES study [22]. In the Vitamin D Antenatal Asthma Reduction Trial (VDAART), a study of 467 pregnant women from Boston, Massachusetts, maternal plasma MePb and PrPb levels were lowest among non-Hispanic White participants, similar to our findings [24]. Likewise, urinary MePb, EtPb, and PrPb were higher among Hispanic participants and those with other racial/ethnic identities than among White participants in the MARBLES study, and PrPb levels were greater among those with less education [23]. In parallel to our findings among pregnant people, urinary MePb and PrPb concentrations were higher among U.S. non-Hispanic Black, Mexican American, and Other Hispanic participants than among non-Hispanic White participants in 1999–2014, and the differences could not be attributed to socioeconomic position [44].
The results of the current study in a large sample of pregnant people underscore the widespread nature of racial and ethnic differences in urinary EP concentrations, despite decreases in exposure to most EPs in all racial/ethnic groups over time [46].
Drivers of racial and ethnic differences in urinary EP concentrations
We found differences in urinary EP concentrations between racial/ethnic groups, primarily reflecting higher urinary concentrations among non-Hispanic Black and Hispanic people than among non-Hispanic White people. Yet, we also found that most urinary EPs were similar for participants with different educational levels. These results suggest that the racial/ethnic differences in urinary EPs were similar among participants with different educational levels, which act as a surrogate for socioeconomic position. Personal care products intended for application to the skin, hair, and nails, as well as deodorizers, fragrances, perfumes, and cleansers, are an important source of exposure to parabens and benzophenones [9, 10, 49, 50]. Use of some personal care products differs among White and non-White women [51,52,53,54]. While preference and product availability are important, the imposition of Eurocentric beauty standards appears to be a key driver of exposure disparities in non-White populations [9, 51, 55, 56]. Use of products marketed to non-White populations to promote White beauty standards, such as hair relaxers and related haircare products, skin lighteners, and douche/vaginal wash products, can lead to higher EP exposures [12, 57]. Greater use of ethno-targeted beauty products has been associated with increased reproductive health risks [58,59,60]. Similarly, differences in consumption of processed, packaged, and canned foods leads to different EP exposures [45, 61, 62], and different patterns of product consumption during pregnancy may contribute to the exposure difference [63]. Unfortunately, product selection may be constrained by availability and cost [64], in addition to preference, so the success of individual actions to reduce exposure is likely to be limited; policy-level initiatives are necessary to intervene effectively on the exposure disparity [65]. Resolving the racial and ethnic difference in prenatal EP exposure will require intensive study of the exposure sources to inform greater regulatory attention, and investigation of racial and ethnic differences in perinatal outcomes and child health that can be attributed in part to the different levels of exposure.
Strengths and limitations
Our sample size of 4006 pregnant people with 7854 urine specimens provided statistical power to detect important differences in urinary EPs among pregnant people with different self-reported racial/ethnic identities. The results of our sensitivity analyses suggested that neighborhood-level confounding was unlikely to bias the results. However, the limited number of participants who identified as non-Hispanic Asian, Hawaiian, American Indian, Alaskan Native, multiple races, and as other racial and ethnic identities precluded analyses as separate groups. A future investigation with oversampling of pregnant people having these racial and ethnic identities is necessary to characterize EP exposure disparities. There were modest differences in effect estimates for urinary BPA, BPF, and BPS when we excluded the TIDES and NYU CHES studies, but most results were also robust to a leave-one-cohort-out analysis.
We measured multiple urinary EPs, including the newer BPA-analog compounds BPF and BPS. However, urinary EPs have short half-lives in vivo. Intraclass correlations ranged from 0.25 for BPS to 0.95 for EtPb in repeated urinary specimens collected at 2 week intervals in Healthy Start [21], suggesting that individual measures may not represent exposure across gestation for some chemicals. Still, we included multiple urinary measurements in the regression models for many participants. The results were also mostly similar in a sensitivity analysis limited to second-trimester urinary specimens, which may in part reflect higher concentrations of some EPs at delivery (24 samples collected at delivery) [66]. Furthermore, there were a large number of samples with BPF values lower than the LOD. We implemented a censored linear mixed effects model to accommodate the uncertainty due to these values. We also included cohort as a fixed effect in regression models to adjust for differences between ECHO cohorts, including using different laboratories to measure EPs [67].
Conclusions
Our results underscore the disproportionately high levels of exposure to EPs among pregnant racial and ethnic minorities in the U.S. Thus, studies of racial/ethnic differences in perinatal health outcomes should account for differences in chemical exposure.
Data availability
Select de-identified data from the ECHO Program are available through NICHD’s Data and Specimen Hub (DASH). Information on study data not available on DASH, such as some Indigenous datasets, can be found on the ECHO study DASH webpage.
References
Buckley JP, Barrett ES, Beamer PI, Bennett DH, Bloom MS, Fennell TR, et al. Opportunities for evaluating chemical exposures and child health in the United States: the Environmental influences on Child Health Outcomes (ECHO) Program. J Expo Sci Environ Epidemiol. 2020;30:397–419.
Woodruff TJ, Zota AR, Schwartz JM. Environmental chemicals in pregnant women in the United States: NHANES 2003-2004. Environ Health Perspect. 2011;119:878–85.
Gore AC, Chappell VA, Fenton SE, Flaws JA, Nadal A, Prins GS, et al. EDC-2: the Endocrine Society’s second scientific statement on endocrine-disrupting chemicals. Endocr Rev. 2015;36:E1–150.
Yoshida T, Andoh K, Fukuhara M. Urinary 2,5-dichlorophenol as biological index for p-dichlorobenzene exposure in the general population. Arch Environ Contam Toxicol. 2002;43:0481–5.
Dubey D, Sharma V, Pass S, Sawhney A, Stüve O. Para-dichlorobenzene toxicity—a review of potential neurotoxic manifestations. Ther Adv Neurol Disord. 2014;7:177–87.
Mustieles V, Balogh RK, Axelstad M, Montazeri P, Márquez S, Vrijheid M, et al. Benzophenone-3: comprehensive review of the toxicological and human evidence with meta-analysis of human biomonitoring studies. Environ Int. 2023;173:107739.
Mustieles V, D’Cruz SC, Couderq S, Rodríguez-Carrillo A, Fini J-B, Hofer T, et al. Bisphenol A and its analogues: a comprehensive review to identify and prioritize effect biomarkers for human biomonitoring. Environ Int. 2020;144:105811.
Nowak K, Ratajczak–Wrona W, Górska M, Jabłońska E. Parabens and their effects on the endocrine system. Mol Cell Endocrinol. 2018;474:238–51.
Helm JS, Nishioka M, Brody JG, Rudel RA, Dodson RE. Measurement of endocrine disrupting and asthma-associated chemicals in hair products used by Black women. Environ Res. 2018;165:448–58.
Dodson RE, Nishioka M, Standley LJ, Perovich LJ, Brody JG, Rudel RA. Endocrine disruptors and asthma-associated chemicals in consumer products. Environ Health Perspect. 2012;120:935–43.
Bloom MS, Varde M, Newman RB. Environmental toxicants and placental function. Best Pract Res Clin Obstet Gynaecol. 2022;85:105–20.
Zota AR, Shamasunder B. The environmental injustice of beauty: framing chemical exposures from beauty products as a health disparities concern. Am J Obstet Gynecol. 2017;217:418.e1–418.e6.
Burris HH, Hacker MR. Birth outcome racial disparities: a result of intersecting social and environmental factors. Semin Perinatol. 2017;41:360–6.
Osterman MJK, Hamilton BE, Martin JA, Driscoll AK, Valenzuela CP. Births: Final Data for 2022. Natl Vital- Stat Rep. 2024;73:1–56.
Ye XY, Wong LY, Zhou XL, Calafat AM. Urinary concentrations of 2,4-dichlorophenol and 2,5-dichlorophenol in the US population (National Health and Nutrition Examination Survey, 2003-2010): trends and predictors. Environ Health Perspect. 2014;122:351–5.
Lehmler H-J, Liu B, Gadogbe M, Bao W. Exposure to bisphenol A, bisphenol F, and bisphenol S in U.S. adults and children: the National Health and Nutrition Examination Survey 2013–2014. ACS Omega. 2018;3:6523–32.
Calafat AM, Ye X, Wong L-Y, Bishop AM, Needham LL. Urinary concentrations of four parabens in the U.S. population: NHANES 2005–2006. Environ Health Perspect. 2010;118:679–85.
Calafat AM, Kuklenyik Z, Reidy JA, Caudill SP, Ekong J, Needham LL. Urinary concentrations of bisphenol A and 4-nonylphenol in a human reference population. Environ Health Perspect. 2005;113:391–5.
Calafat AM, Wong LY, Ye XY, Reidy JA, Needham LL. Concentrations of the sunscreen agent benzophenone-3 in residents of the United States: National Health and Nutrition Examination Survey 2003-2004. Environ Health Perspect. 2008;116:893–7.
Mortensen ME, Calafat AM, Ye XY, Wong LY, Wright DJ, Pirkle JL, et al. Urinary concentrations of environmental phenols in pregnant women in a pilot study of the National Children’s Study. Environ Res. 2014;129:32–8.
Polinski KJ, Dabelea D, Hamman RF, Adgate JL, Calafat AM, Ye XY, et al. Distribution and predictors of urinary concentrations of phthalate metabolites and phenols among pregnant women in the Healthy Start Study. Environ Res. 2018;162:308–17.
Aung MT, Ferguson KK, Cantonwine DE, McElrath TF, Meeker JD. Preterm birth in relation to the bisphenol A replacement, bisphenol S, and other phenols and parabens. Environ Res. 2019;169:131–8.
Kim K, Shin H-M, Busgang SA, Barr DB, Panuwet P, Schmidt RJ, et al. Temporal trends of phenol, paraben, and triclocarban exposure in California pregnant women during 2007–2014. Environ Sci Technol. 2021;55:11155–65.
Lee-Sarwar K, Hauser R, Calafat AM, Ye X, O’Connor GT, Sandel M, et al. Prenatal and early-life triclosan and paraben exposure and allergic outcomes. J Allergy Clin Immunol. 2018;142:269–278.e15.
James-Todd TM, Chiu Y-H, Zota AR. Racial/ethnic disparities in environmental endocrine disrupting chemicals and women’s reproductive health outcomes: epidemiological examples across the life course. Curr Epidemiol Rep. 2016;3:161–80.
Chan M, Mita C, Bellavia A, Parker M, James-Todd T. Racial/ethnic disparities in pregnancy and prenatal exposure to endocrine-disrupting chemicals commonly used in personal care products. Curr Environ Health Rep. 2021;8:98–112.
Knapp EA, Kress AM, Parker CB, Page GP, McArthur K, Gachigi KK, et al. The environmental influences on child health outcomes (ECHO)-wide cohort. Am J Epidemiol. 2023;192:1249–63.
Cerdeña JP, Grubbs V, Non AL. Genomic supremacy: the harm of conflating genetic ancestry and race. Hum Genom. 2022;16:18.
Payne-Sturges DC, Gee GC, Cory-Slechta DA. Confronting racism in environmental health sciences: moving the science forward for eliminating racial inequities. Environ Health Perspect. 2021;129:55002.
Chandran A, Knapp E, Liu T, Dean LT. A new era: improving use of sociodemographic constructs in the analysis of pediatric cohort study data. Pediatr Res. 2021;90:1132–8.
Autor DH. Skills, education, and the rise of earnings inequality among the “other 99 percent.” Science 2014;344:843–51.
Flanagan BE, Gregory EW, Hallisey EJ, Heitgerd JL, Lewis B. A social vulnerability index for disaster management. J. Homel. Secur Emergency Manag. 2011;8:3.
Hornung RW, Reed LD. Estimation of average concentration in the presence of nondetectable values. Appl Occup Environ Hyg. 1990;5:46–51.
Boeniger MF, Lowry LK, Rosenberg J. Interpretation of urine results used to assess chemical exposure with emphasis on creatinine adjustments: a review. Am Ind Hyg Assoc J. 1993;54:615–27.
Kuiper JR, O’Brien KM, Welch BM, Barrett ES, Nguyen RHN, Sathyanarayana S, et al. Combining urinary biomarker data from studies with different measures of urinary dilution. Epidemiology. 2022;33:533–40.
Vaida F, Liu L. Fast implementation for normal mixed effects models with censored response. J Comput. Graph Stat. 2009;18:797–817.
Rizopoulos D. GLMMadaptive [Internet]. 2023. Available from: https://cran.r-project.org/web/packages/GLMMadaptive/index.html
VanderWeele TJ. Principles of confounder selection. Eur J Epidemiol. 2019;34:211–9.
Howe CJ, Bailey ZD, Raifman JR, Jackson JW. Recommendations for using causal diagrams to study racial health disparities. Am J Epidemiol. 2022;191:1981–9.
Bland JM, Altman DG. Multiple significance tests: the Bonferroni method. BMJ. 1995;310:170.
Takahashi O, Oishi S, Yoneyama M, Ogata A, Kamimura H. Antiestrogenic effect of paradichlorobenzene in immature mice and rats. Arch Toxicol. 2007;81:505–17.
Pridgen GW, Zhu J, Wei Y. Exposure to p-dichlorobenzene and prevalent endocrine-related reproductive cancers among US women. Environ Sci Pollut Res. 2023;30:78324–31.
Baker BH, Wu H, Laue HE, Boivin A, Gillet V, Langlois M-F, et al. Methylparaben in meconium and risk of maternal thyroid dysfunction, adverse birth outcomes, and Attention-Deficit Hyperactivity Disorder (ADHD). Environ Int. 2020;139:105716.
Nguyen VK, Kahana A, Heidt J, Polemi K, Kvasnicka J, Jolliet O, et al. A comprehensive analysis of racial disparities in chemical biomarker concentrations in United States women, 1999–2014. Environ Int. 2020;137:105496.
van Woerden I, Payne-Sturges DC, Whisner CM, Bruening M. Dietary quality and bisphenols: trends in bisphenol A, F, and S exposure in relation to the Healthy Eating Index using representative data from the NHANES 2007–2016. Am J Clin Nutr. 2021;114:669–82.
Stanfield Z, Setzer RW, Hull V, Sayre RR, Isaacs KK, Wambaugh JF. Characterizing chemical exposure trends from NHANES urinary biomonitoring data. Environ Health Perspect. 2024;132:017009.
Calafat AM, Longnecker MP, Koch HM, Swan SH, Hauser R, Goldman LR, et al. Optimal exposure biomarkers for nonpersistent chemicals in environmental epidemiology. Environ Health Perspect. 2015;123:A166–8.
Nethery E, Brauer M, Janssen P. Time-activity patterns of pregnant women and changes during the course of pregnancy. J Expo Sci Environ Epidemiol. 2009;19:317–24.
Branch F, Woodruff TJ, Mitro SD, Zota AR. Vaginal douching and racial/ethnic disparities in phthalates exposures among reproductive-aged women: National Health and Nutrition Examination Survey 2001–2004. Environ Health. 2015;14:1–8.
Liao C, Kannan K. Widespread occurrence of benzophenone-type UV light filters in personal care products from China and the United States: An assessment of human exposure. Environ Sci Technol. 2014;48:4103–9.
Dodson RE, Cardona B, Zota AR, Robinson Flint J, Navarro S, Shamasunder B. Personal care product use among diverse women in California: Taking Stock Study. J Expo Sci Environ Epidemiol. 2021;31:487–502.
Zota AR, Franklin ET, Weaver EB, Shamasunder B, Williams A, Siegel EL, et al. Examining differences in menstrual and intimate care product use by race/ethnicity and education among menstruating individuals. Front Reprod Health. 2023;5:286920.
Llanos AAM, Rockson A, Getz K, Greenberg P, Portillo E, McDonald JA, et al. Assessment of personal care product use and perceptions of use in a sample of US adults affiliated with a university in the Northeast. Environ Res. 2023;236:116719.
Payne CE, Rockson A, Ashrafi A, McDonald JA, Bethea TN, Barrett ES, et al. Beauty beware: associations between perceptions of harm and safer hair-product-purchasing behaviors in a cross-sectional study of adults affiliated with a university in the Northeast. Int J Environ Res Public Health. 2023;20:7129.
McDonald JA, Llanos AAM, Morton T, Zota AR. The environmental injustice of beauty products: toward clean and equitable beauty. Am J Public Health. 2022;112:50–3.
Berger KP, Kogut KR, Bradman A, She J, Gavin Q, Zahedi R, et al. Personal care product use as a predictor of urinary concentrations of certain phthalates, parabens, and phenols in the HERMOSA study. J Expo Sci Environ Epidemiol. 2019;29:21–32.
Edwards L, Ahmed L, Martinez L, Huda S, Shamasunder B, McDonald JA, et al. Beauty inside out: Examining beauty product use among diverse women and femme-identifying individuals in northern Manhattan and south Bronx through an environmental justice framework. Environ Justice. 2023;16:449–60.
Wise L, Wang T, Ncube C, Lovett S, Abrams J, Boynton-Jarrett R, et al. Use of chemical hair straighteners and fecundability in a North American preconception cohort. Am J Epidemiol. 2023;192:1066–80.
Chang C, O’Brien K, Keil A, Gaston S, Jackson C, Sandler D, et al. Use of straighteners and other hair products and incident uterine cancer. J Natl Cancer Inst. 2022;114:1636–45.
Chan M, Preston EV, Fruh V, Quinn MR, Hacker MR, Wylie BJ, et al. Use of personal care products during pregnancy and birth outcomes—a pilot study. Environ Res. 2023;225:115583.
Muncke J. Exposure to endocrine disrupting compounds via the food chain: Is packaging a relevant source? Sci Total Environ. 2009;407:4549–59.
Buckley JP, Kim H, Wong E, Rebholz CM. Ultra-processed food consumption and exposure to phthalates and bisphenols in the US National Health and Nutrition Examination Survey, 2013–2014. Environ Int. 2019;131:105057.
Sterrett ME, Bloom MS, Jamro EL, Wenzel AG, Wineland RJ, Unal ER, et al. Maternal food and beverage consumption behaviors and discrepant phthalate exposure by race. Int J Environ Res Public Health. 2021;18:2190.
Chan M, Parikh S, Shyr D, Shamasunder B, Adamkiewicz G, James-Todd T. Evaluating neighborhood-level differences in hair product safety by environmental working group ratings among retailers in Boston, Massachusetts. Environ Health Perspect. 2023;131:97002.
Yang TC, Jovanovic N, Chong F, Worcester M, Sakhi AK, Thomsen C, et al. Interventions to reduce exposure to synthetic phenols and phthalates from dietary intake and personal care products: a scoping review. Curr Environ Health Rep. 2023;10:184–214.
Vandentorren S, Zeman F, Morin L, Sarter H, Bidondo M-L, Oleko A, et al. Bisphenol-A and phthalates contamination of urine samples by catheters in the Elfe pilot study: Implications for large-scale biomonitoring studies. Environ Res. 2011;111:761–4.
Basagaña X, Pedersen M, Barrera-Gómez J, Gehring U, Giorgis-Allemand L, Hoek G, et al. Analysis of multicentre epidemiological studies: contrasting fixed or random effects modelling and meta-analysis. Int J Epidemiol. 2018;47:1343–54.
Acknowledgements
The authors wish to thank our ECHO Colleagues; the medical, nursing, and program staff; and the children and families participating in the ECHO cohort. We would also like to thank Diana Steele Jones for outstanding editorial assistance. Research reported in this publication was supported by the Environmental influences on Child Health Outcomes (ECHO) Program, Office of the Director, National Institutes of Health, under Award Numbers U2COD023375 (Coordinating Center), U24OD023382 (Data Analysis Center), U24OD023319 with co-funding from the Office of Behavioral and Social Science Research (Measurement Core), U24OD035523 (Lab Core), ES0266542 (HHEAR), U24ES026539 (HHEAR Barbara O’Brien), U2CES026533 (HHEAR Lisa Peterson), U2CES026542 (HHEAR Patrick Parsons, Kannan Kurunthachalam), U2CES030859 (HHEAR Manish Arora), U2CES030857 (HHEAR Timothy R. Fennell, Susan J. Sumner, Xiuxia Du), U2CES026555 (HHEAR Susan L. Teitelbaum), U2CES026561 (HHEAR Robert O. Wright), U2CES030851 (HHEAR Heather M. Stapleton, P. Lee Ferguson), UG3/UH3OD023251 (Akram Alshawabkeh), UH3OD023320 and UG3OD035546 (Judy Aschner), UH3OD023332 (Clancy Blair, Leonardo Trasande), UG3/UH3OD023253 (Carlos Camargo), UG3/UH3OD023248 and UG3OD035526 (Dana Dabelea), UG3/UH3OD023313 (Daphne Koinis Mitchell), UH3OD023328 (Cristiane Duarte), UH3OD023318 (Anne Dunlop), UG3/UH3OD023279 (Amy Elliott), UG3/UH3OD023289 (Assiamira Ferrara), UG3/UH3OD023282 (James Gern), UH3OD023287 (Carrie Breton), UG3/UH3OD023365 (Irva Hertz-Picciotto), UG3/UH3OD023244 (Alison Hipwell), UG3/UH3OD023275 (Margaret Karagas), UH3OD023271 and UG3OD035528 (Catherine Karr), UH3OD023347 (Barry Lester), UG3/UH3OD023389 (Leslie Leve), UG3/UH3OD023344 (Debra MacKenzie), UH3OD023268 (Scott Weiss), UG3/UH3OD023288 (Cynthia McEvoy), UG3/UH3OD023342 (Kristen Lyall), UG3/UH3OD023349 (Thomas O’Connor), UH3OD023286 and UG3OD035533 (Emily Oken), UG3/UH3OD023348 (Mike O’Shea), UG3/UH3OD023285 (Jean Kerver), UG3/UH3OD023290 (Julie Herbstman), UG3/UH3OD023272 (Susan Schantz), UG3/UH3OD023249 (Joseph Stanford), UG3/UH3OD023305 (Leonardo Trasande), UG3/UH3OD023337 (Rosalind Wright), UG3OD035508 (Sheela Sathyanarayana), UG3OD035509 (Anne Marie Singh), UG3OD035513 and UG3OD035532 (Annemarie Stroustrup), UG3OD035516 and UG3OD035517 (Tina Hartert), UG3OD035518 (Jennifer Straughen), UG3OD035519 (Qi Zhao), UG3OD035521 (Katherine Rivera-Spoljaric), UG3OD035527 (Emily S Barrett), UG3OD035540 (Monique Marie Hedderson), UG3OD035543 (Kelly J Hunt), UG3OD035537 (Sunni L Mumford), UG3OD035529 (Hong-Ngoc Nguyen), UG3OD035542 (Hudson Santos), UG3OD035550 (Rebecca Schmidt), UG3OD035536 (Jonathan Slaughter), UG3OD035544 (Kristina Whitworth). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The sponsor, NIH, participated in the overall design and implementation of the ECHO Program, which was funded as a cooperative agreement between NIH and grant awardees. The sponsor approved the Steering Committee-developed ECHO protocol and its amendments including COVID-19 measures. The sponsor had no access to the central database, which was housed at the ECHO Data Analysis Center. Data management and site monitoring were performed by the ECHO Data Analysis Center and Coordinating Center. All analyses for scientific publication were performed by the study statistician, independently of the sponsor. The lead author wrote all drafts of the manuscript and made revisions based on co-authors and the ECHO Publications Committee (a subcommittee of the ECHO Operations Committee) feedback without input from the sponsor. The study sponsor did not review or approve the manuscript for submission to the journal. Drs. Bloom and Wosu had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Consortia
Contributions
MSB conceived the study, interpreted the data, drafted the manuscript and led the writing, and approved the final version for submission; SU analyzed the data, revised the manuscript, and approved the final version for submission; AWN interpreted the data, revised the manuscript, and approved the final version for submission; JRK interpreted the data, revised the manuscript, and approved the final version for submission; JPB interpreted the data, revised the manuscript, and approved the final version for submission; JA designed the study, revised the manuscript, and approved the final version for submission; DB designed the study, revised the manuscript, and approved the final version for submission, ESB designed the study, revised the manuscript, and approved the final version for submission; DHB designed the study, revised the manuscript, and approved the final version for submission; DD designed the study, revised the manuscript, and approved the final version for submission; ALD designed the study, revised the manuscript, and approved the final version for submission; AF interpreted the data, revised the manuscript, and approved the final version for submission; MK designed the study, revised the manuscript, and approved the final version for submission; DL interpreted the data, revised the manuscript, and approved the final version for submission; JM designed the study, revised the manuscript, and approved the final version for submission; RM designed the study, revised the manuscript, and approved the final version for submission; TGO designed the study, revised the manuscript, and approved the final version for submission; MER interpreted the data, revised the manuscript, and approved the final version for submission; SS designed the study, revised the manuscript, and approved the final version for submission; APS interpreted the data, revised the manuscript, and approved the final version for submission; AmS designed the study, revised the manuscript, and approved the final version for submission; DJW designed the study, revised the manuscript, and approved the final version for submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
All data collection and research methods were approved by IRBs at each cohort site and the ECHO Data Analysis Center, and all participants provided written informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bloom, M.S., Upadhyaya, S., Nzegwu, A.W. et al. Racial and ethnic differences in prenatal exposure to environmental phenols and parabens in the ECHO Cohort. J Expo Sci Environ Epidemiol (2025). https://doi.org/10.1038/s41370-025-00750-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41370-025-00750-w